Can you ever ‘fix’ your Pelvic Organ Prolapse - Every thing you need to know about living with pelvic organ prolapse
Prolapse can steal so much from us. From chasing your child in the park or dancing at a friend’s wedding. To carrying your baby in a sling. Simple moments become tinged with doubt.
Our body’s foundation feels weak. And so we grip. We contract. We try our best to hold on (and to hold in). And in this contraction, we start to lose ourselves. We become defined by a condition that is hard to explain and difficult to talk about.
If you are living with pelvic organ prolapse we want you to know you are not alone.
And while the first stages of prolapse recovery can feel overwhelming and frustrating, there is hope. You won’t feel like this forever. Your body will grow stronger and your prolapse will play a smaller role in your life and in your thoughts.
We hope that by reading this post you feel less alone, more hopeful and more empowered to take the steps you need on your healing journey.
Contents
- First things first, what is Pelvic Organ Prolapse
- The Emotional Toll of Living with Prolapse
- Types of Prolapse
- Prolapse Stages
- What causes Prolapse
- Can you Heal your Prolapse
- Pelvic Floor Muscle Training and Prolapse
- Other Steps for Healing Pelvic Organ Prolapse
- Exercise and Prolapse
- Pessaries
- Pregnancy and Prolapse
- Prolapse and Subsequent Births
- Running with Prolapse
- Should I consider surgery?

First things first, what is Pelvic Organ Prolapse
Prolapse is a hernia, and the hernial portal is the ‘levator hiatus’ (ie the opening in the pelvic floor muscle or ‘levator ani’, which allows the urethra, vagina and rectum to pass through). The Royal Australian College of General Practitioners defines a pelvic organ prolapse "as the downward displacement of pelvic organs, resulting in herniation of those organs into or through the vagina (uterovaginal prolapse) or anal canal (in the case of rectal intussusception and rectal prolapse).
Prolapse diagnosis can feel overwhelming because of this one simple fact. For most women, the first time they hear the phrase ‘pelvic organ prolapse’ is when they are being diagnosed with one. Despite close to 50% of women living with some form of pelvic organ prolapse or pelvic floor dysfunction, it is still considered a taboo topic, and one that is often only spoken about by the brave. (Palmieri et al 2022)
Prolapse can happen for a variety of reasons and it is often a combination of factors that leads to prolapse. Pregnancy, the type of birth you had, history of chronic constipation, genetics, biomechanics, hormones, weight and a history of high impact movement can all contribute to prolapse.
You are Not Alone! Some statistics surrounding prolapse
- Close to 50% of women will be defined as having a non-clinical prolapse, with only 15 -30% of these women experiencing associated symptoms.
- The biggest risk increase in a woman’s life for prolapse is her first birth, which gives almost a 10-fold increase in risk. (Quiroz et al. 2010))
- There is a lifetime risk of 10 – 20% for women needing prolapse surgery (Smith et al. 2010)
- Women wait, on average, 33 years before presenting for surgery for prolapse following their first birth. ( Thomas et al. 2015)
- Women who give birth via forceps delivery have a 53% chance of having significant defects in their pelvic floor muscles called levator avulsion. ( Dietz et al. 2015)
- Women who have given birth via forceps have a significantly increased prolapse risk than a normal vaginal delivery (Olloyhaug et al. 2015, Dietz 2015)
For some, a prolapse might feel like a heaviness or dragging in the vagina. It may feel like you are constantly wearing a pad or have a golf ball stuck in your vagina. The common symptoms of prolapse also include a vaginal lump or bulge (whether visible or not), a dragging sensation, feelings of vaginal laxity or looseness and pain before, during or after vaginal intercourse.
There may also be a range of accompanying conditions such as urinary incontinence, straining to void or intermittent stream, trouble having bowel motions or incomplete emptying, recurrent urinary tract infections and pain or lack of sensation during sex.
If you are concerned about any of the above symptoms, don't hesitate to get in touch with your healthcare professional.

The Emotional Toll of Living with Prolapse
Before we move on to your physical recovery, it is important to acknowledge the emotional toll of living with prolapse. Prolapse is much more than 'just' a physical condition. It affects every area of your well-being - mental, emotional, sexual and social. Having supported thousands of women with prolapse through the Empowered Motherhood Program, we know that for a lot of women, the way women receive their prolapse diagnosis often leaves them with a distinct lack of hope. They will often be given a long list of exercises to avoid, along with the distinct feeling that their quality of life will be forever impacted.
Right now, you may feel like your body has failed you. You might feel a little broken or that your old life has been whipped out from under you.
We are here to remind you that you aren't broken, your body hasn't failed you, and you definitely didn't cause your prolapse. You can live a healthy, active life with prolapse with the right treatment and support.
Living with prolapse is an incredibly humbling experience full of deep learning. It will teach you to respect your body and its limits. It will help you better understand the intricate link between your breath, energy, stress and physical symptoms. It will teach you to greater humility and inner strength. Whilst your prolapse might feel all-consuming right now, there will come a time when your symptoms don’t dictate your life. Whether this is because your symptoms have drastically improved, or because you have learned to accept them as a part of your life, things will get better.
If you want to read about how Jen turned her prolapse diagnosis into an incredible online community that supports other women living with pop - you can read her story here.
Types of Prolapse
There are several types of pelvic organ prolapse, which are classified based on which organ or structure is affected. The four most common types of pelvic organ prolapse are:
- Anterior compartment Prolapse: This type of prolapse occurs when the bladder or urethra shifts downwards and protrudes into the front wall of the vagina ( Historically referred to as Cystocele and urethrocele).
- Posterior Compartment Prolapse: In this type of prolapse, the rectum bulges forward and pushes against the back wall of the vagina. ( Historically referred to as a Rectocele)*
- Central Compartment Prolapse: This type of prolapse happens when the uterus and cervix descend and presses against the vaginal opening (Uterine or cervix prolapse)
- Vaginal vault Prolapse: This type of prolapse occurs when the top of the vagina loses support and falls downward into the vaginal cavity after a hysterectomy.
A less common form of posterior wall Prolapse that occurs in the upper portion is when the part of the small intestine protrudes into the upper vaginal canal. This historically was referred to as an 'enterocele.'
We can’t say this enough—if you are experiencing any symptoms of prolapse, please don’t self-diagnose. Get support from a qualified pelvic health physiotherapist, obstetrician, or gynaecologist. You can see our list of Pelvic Health Physiotherapists throughout Australia here.
Prolapse Stages
The stages of pelvic organ prolapse are classified according to the degree of descent or protrusion of the affected organ(s). The International Continence Society (ICS) has developed a staging system that ranges from stage 0 to stage 4:
- Stage 1: Very mild prolapse – organs are still fairly well supported by the pelvic floor (the most distended part is more than 1cm above the hymen).
- Stage 2: Moderate prolapse. Pelvic floor organs have begun to descend but are still contained inside the vagina (the most distended part is between 1cm above and 1cm below the hymen)
- Stage 3: Severe prolapse. Pelvic floor organs have descended to or beyond the opening of the vagina (the most distended part is more than 1 cm below the hymen).
- Stage 4: Complete prolapse. Pelvic floor organs descended completely through the vaginal opening so that the entire organ is outside of the vagina (complete descent).
Something important to note is that multiple studies show if we were to examine a group of women that were an average age of 22, that had not yet had a baby that, 40-50% of them would actually be defined as having a stage one prolapse.
And as none of these women reported feeling a heaviness or bulge in the vagina, it has led many to conclude that stage one Pelvic organ prolapse is actually NORMAL anatomy and should not be considered prolapse ( Bushbaum et al. 2006)
As a result, there is a consensus and a new classification to be defined as “ Clinical Pelvic Organs Prolapse.”
Clinical Pelvic Organ Prolapse
A 'clinical pelvic organ prolapse' is the anatomical prolapse with the descent of at least one of the vaginal walls to or beyond the vaginal hymen with maximal Valsalva effort WITH the presence either of bothersome characteristic symptoms, most commonly the sensation of vaginal bulge or of functional or medical compromise due to prolapse without symptom bother." (Colins et al 2021)
So, the symptoms of prolapse are just as important as what the examination findings show!
What Causes Prolapse
Prolapse can happen for a variety of reasons. Genetic factors, a history of chronic constipation, collagen types, biomechanics, hormones, weight, a history of high-impact movement, pregnancy, and birth can all contribute. There is no single defined reason that one individual will develop prolapse; it is usually a combination of accumulative factors.
We do know that the largest contributing factor, however, is pregnancy and vaginal birth. During pregnancy, the body starts to prepare for what is required during the birth, which is essentially to propel the baby towards the pelvic outlet and allow it to pass through into the world towards its first breath.
The body's inbuilt wisdom knows that in 9 months' time, it will require strong uterine contractions (the preparation for this is Braxton Hicks), an opening of the pelvic bones (the preparation for this is softening of the pelvic ligaments) and an opening of the pelvic outlet (the preparation work is a lengthening and weakening of the pelvic floor).
Once the baby has entered the pelvic outlet and is crowing, the levator ani will then need to stretch up to 3 times its normal length, which is the length at which almost all skeletal muscle would rupture. In most cases, the changes that have occurred during pregnancy allow this to happen without major injury however, in around 10-20% of births, it struggles with this lengthening, reaching its maximum point of stretch before the pelvic floor has to give way, tearing at the bony attachment point (a levator avulsion).
As the levator ani is one of the major organ supports, it’s no surprise that we have strong evidence to show the link between a levator avulsion and risk profile for prolapse. It is important to note that the statistic for levator avulsion actually increases to 30 - 65% when forceps are required during labour. (Dietz et al 2005).
Of course, there is more to a prolapse than simply a weakened or damaged pelvic floor. Other factors, such as poor biomechanics and movement patterns, an inability to manage and distribute pressure throughout the core canister and increased tension or tightness in other areas of the body can all contribute to the development of pelvic organ prolapse over the long term.
You are not to blame for your prolapse.
It is really important for your healing to understand that you are not responsible for your prolapse. No single act or choice on your part led to this condition. And just like no one factor caused your prolapse, no one factor will help you heal it.
Understanding the factors that may have contributed to your prolapse as an individual is valuable in order to heal as well as possible. However, blaming yourself for any actions you took in the past can also lead to feelings of guilt, regret, and sadness. These are unnecessary and not helpful.
Our joint experience shows us that the best outcomes come when you keep looking forward and focusing on everything you CAN do to help your pelvic floor function and your pelvic organs feel more supported.
In the Empowered Motherhood Program, we incorporate the tools below for healing into each of our workouts. So that every time you move, you are healing your body and strengthening your mind.
- Proper breathing.
- Optimal posture.
- Optimal pelvic floor safe movement patterns.
- Mental and emotional support.
- Core and pelvic floor strength.
- Pressure regulation and core control.
- Creating full-body strength.
- Introducing impact safely.

Can you Heal your Prolapse?
Some of the most common questions we get asked in the Empowered Motherhood Program are:
- Will I always feel like this?
- Is it going to get better for me?
- Can I fix this?
When we think about the postnatal body, how your body feels, functions and looks six weeks postnatal is completely different to how it functions, feels and looks 12 months + after birth. Likewise, how your pelvic floor looks and feels in the early stages of your postnatal recovery is completely different to how it will look and feel when you are 18 months postpartum. The pelvic floor and pelvic organs need time to heal and return toward their normal range of movement and place within the body.
According to the prolapse classifications, many women who present for internal assessments at six weeks postnatal would be considered to have pelvic organ prolapse. However, at 6 weeks postnatal, your body is still in a physiological and anatomical altered state. If we look at these same women at a later point in their postnatal journey, for many women, the prolapse has significantly improved or no longer exists.
So if you are newly postnatal and have been diagnosed with a prolapse, with the right treatment and support, how you feel now will be very different to how you will feel in 12-18 months. And whilst that time frame may seem frustratingly long, prolapse recovery is not a quick journey. It requires patients and consistent work. But the long-term pay-off is definitely worth it!
The degree of recovery you may experience will depend on a number of factors. These include:
- Body Type—Your body type will affect your rate of recovery. Everything from body shape to muscle bulk and connective tissue will affect rates and degrees of healing.
- Connective Tissue Types—Our bodies have different types and ratios of connective tissue, some of which create more rigidity or others of which create more elasticity. These ratios can affect the amount of organ support provided at rest and the degree of distensibility.
- Pelvic floor Muscle Weakness - The levator ani forms an important role in supporting the organs. When the pelvic floor muscles are weaker and not functioning well, this can reduce support and increase the risk of prolapse.
- Pelvic floor Muscle Damage—As the baby crowns and passes through the pelvic outlet, it is not uncommon for the pelvic floor muscle to undergo micro or macro trauma (an avulsion). When this occurs, there is a deep tear in the attachment point of part of the pelvic floor to the pubic bone, which is unfortunately irreversible. This tear results in an increased hiatus width and increased prolapse risk.
- Endovaginal Fascial Damage - Between each organ is a strong web of fascia that supports and helps to suspend the organs. When this is damaged or overstretch, the degree of support reduces.
- Biomechanics and Load Management - How well you move in daily life and place loads through the abdominal and pelvic area can play a role in prolapse symptoms, especially with respect to intra-abdominal pressure.
- Weight, Diet, and Fatigue—Prolapse recovery takes a whole-body approach, and this includes optimising diet, reaching a healthy weight range, managing stress, and ensuring you are getting enough rest and downtime.
- Family History - If you have a family history of prolapse, research shows us you are likely to have an increased risk of prolapse. There are many possible reasons, but the most likely would be a genetic predisposition due to body type and connective tissue.
It is important to have hope, but we also believe it is important to be realistic. Whilst you might not be able to completely heal your prolapse in the sense of your body and pelvic floor returning to it’s pre-pregnancy state, there is so much you can do to reduce your symptoms and improve your quality of life.
The postpartum or postmenopausal body is forever changed. And whilst we would love to tell you that you can fix your prolapse, the truth is that you are probably always going to live with some degree of increased movement in your pelvic organs. And you will probably always have to be more mindful of your pelvic floor than you were pre-children. However, some steps can be taken to manage your symptoms and prevent further progression.

Pelvic Floor Muscle Training and Prolapse
Prolapse isn’t caused solely by a weak pelvic floor, and Kegels aren’t the only answer. However, the research shows that strengthening the pelvic floor muscles through pelvic floor muscle training (PFMT) can be an effective non-surgical treatment option for managing the symptoms of pelvic organ prolapse.
A 2021 systematic review and meta-analysis of randomized controlled trials found that PFMT effectively reduced prolapse symptoms and improved the quality of life for women with pelvic organ prolapse. The review also found that longer durations of PFMT and supervised programs were associated with greater improvement in prolapse symptoms. (Hagen et all 2021).
A 2020 randomized controlled trial found that a combination of pelvic floor muscle training and behavioral therapy (where skills to help alter and improve behavior are taught) was more effective in reducing prolapse symptoms compared to pelvic floor muscle training alone. The study also found that women who received the combination therapy were more likely to continue with treatment and have better long-term outcomes. (Hung et al 2020).
Another study published in 2020 found that pelvic floor muscle training can improve pelvic organ support and reduce the severity of prolapse in women with early-stage pelvic organ prolapse. Soave, I et al 2020).
Overall, the latest research suggests that pelvic floor muscle training can be an effective non-surgical treatment option for managing pelvic organ prolapse. However, the effectiveness of PFMT may vary depending on the severity and type of prolapse, and treatment options should be individualized based on specific needs and symptoms.
Other Steps for Healing Pelvic Organ Prolapse
Healing prolapse takes a whole-body and mind approach. In addition to your pelvic floor muscle training, the following factors will contribute to your prolapse recovery.
- Maintaining a healthy weight: Excess weight can put additional pressure on the pelvic organs and weaken the supporting muscles, which can contribute to prolapse. Where it is possible you, maintaining a healthy weight through a balanced diet and regular exercise can help reduce the risk of prolapse or prevent further progression, especially in the case of posterior wall prolapses.
- Avoiding heavy lifting with poor technique: Lifting heavy objects can strain the pelvic muscles and exacerbate symptoms of prolapse. It is important to train your body to lift heavy objects and weights well. This may involve re-training motor patterns and breathing strategies as well as being more mindful in your day-to-day life of the impact of lifting heavy items.
- Treating constipation: Treating constipation: Straining during bowel movements can put a large amount of pressure on the pelvic organs and can worsen prolapse symptoms. Eating a high-fibre diet, staying hydrated, using stool softeners or laxatives, and learning to defecate correctly can reduce the straining and load during bowel movements.
- Sleep and Immunity: Chronic coughing can significantly affect your ability to heal. And whilst gettgin sick is a part of life, investing in your immune health and ensuring that you are getting as much sleep as you can (especilaly if you are in those early postpartum days) will support your prolapse recovery.
- Full Body Strength: Building full body strength will result in less load being transferred through your core and pelvic floor. So ensure that you are doing at least 2 pelvic floor safe full body strength sessions a week.
- Using pessaries: A pessary is a medical-grade silicone device that is inserted into the vagina to provide support for the pelvic organs. It can be a temporary or long-term solution for managing prolapse symptoms.
Exercise and Prolapse
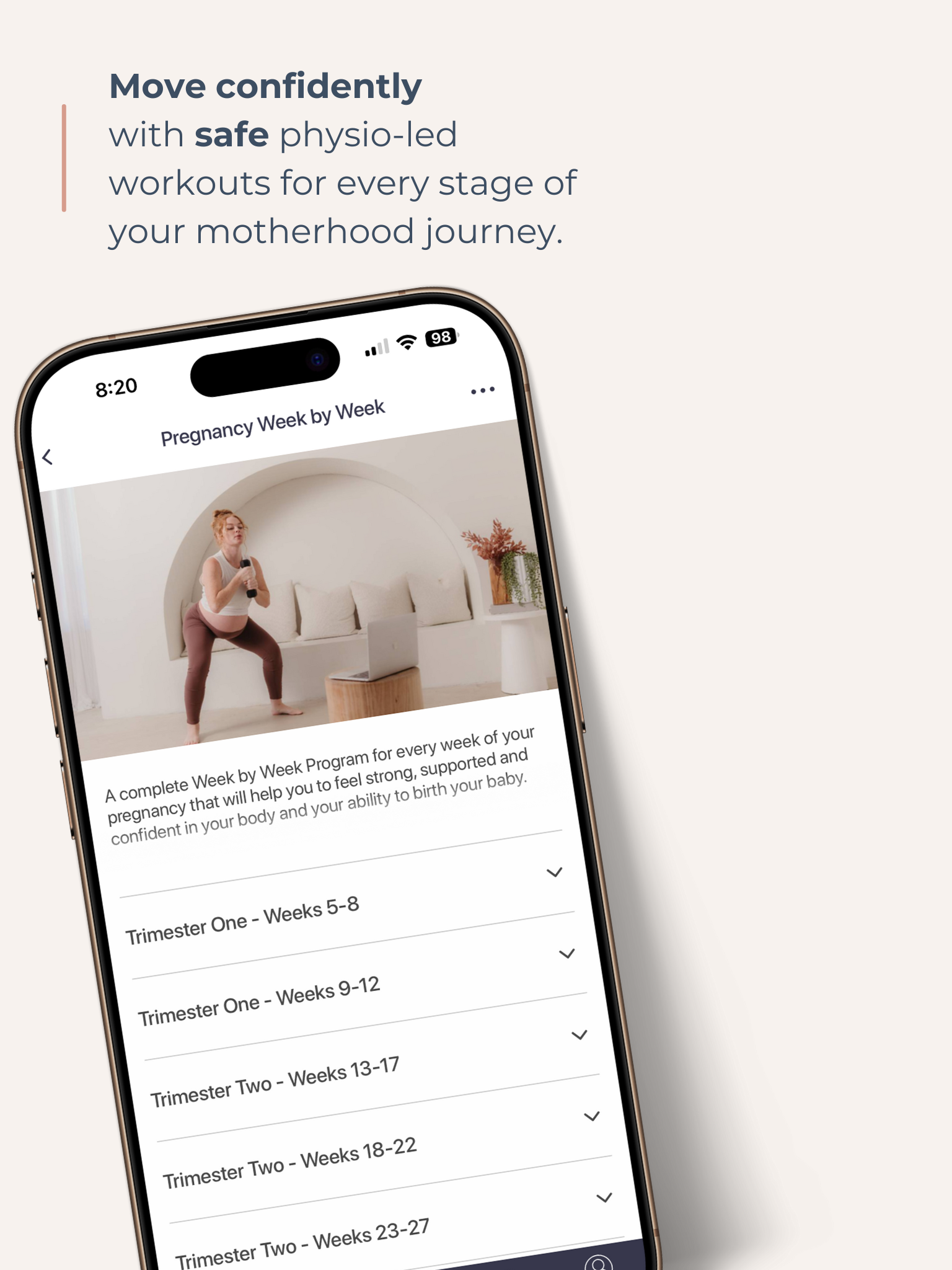
In the Empowered Motherhood Program, we are passionate about helping women with POP to be able to exercise safely and to feel strong, connected and in control of their bodies. We do this through our Prolapse Safe Program which combines education and personal insights together with POP Safe pilates, strength and cardio workouts to help you to return to exercise safely and confidently. You can see more about our Pelvic Floor Safe Week by Week Program here. We believe that with the right movement patterns and technique, almost all forms of exercise can be done safely with prolapse.
When we consider general advice for postnatal recovery, we need to acknowledge that every woman or birthing person is different. And how they will recover will depend on a myriad of factors, including their birth, how much sleep they are getting, their level of general health and fitness, their body type, how much support they have and whether they experienced physical or emotional birth trauma.
If you haven’t already, we recommend watching the short video above to help you return to exercise with prolapse safely.
In the EMP, we focus on the following approach to prolapse-safe exercise:
1. Pelvic Floor Recovery 101
No matter how you gave birth, your postpartum recovery starts with your pelvic floor. As you may know, one role of the pelvic floor is to support the pelvic organs. A second role is to create a tight seal or ‘sphincter’ around the urethra and rectum to prevent incontinence. In its weakened and stretched state, the pelvic floor may not perform either of these roles well.
If you gave birth vaginally, your pelvic floor may have had to stretch up to 3 times its normal length to allow for your baby’s head to pass through. It’s no wonder that studies show an average of 25 – 35% reduction in pelvic floor strength following birth.
If you gave birth via C-Section, you still will have a weakened pelvic floor due to nine months of having to support the extra weight of your uterus, increased blood volume and additional weight!
Our Pelvic Floor programs start with gentle activations designed to reduce inflammation, re-establish neural pathways, support continence and promote the healing of stitches or tears. Our pelvic floor program progresses with you and builds you up to strong and functional pelvic floor exercises designed to help you return to running and impact (hopefully leak-free!).
2. Core Rehabilitation
Your pelvic floor is connected to your core through a complex system of fascia and connective tissue. How your core functions and transfers pressure can directly affect the amount of load that is placed on your pelvic floor. So it is incredibly important to heal your core and build strength and control through your abdominal wall through a safe core rehabilitation program.
In the Empowered Motherhood Program, our Core Connect series will help you to:
- Breathe Well: Learn to breath in a way that supports the natural movement of the abdominal wall and pelvic floor;
- Improve Posture: Our early postnatal classes are designed to help improve mobility and posture so that your abdominal wall and pelvic floor can function optimally.
- Engage your Deep Core: Our physio-led classes are designed to help you properly engage your deepest layer of abdominal muscles, your transversus abdominis (TvA).
- Heal Separation: A mistake that we see women make is that they stick to safe “TvA” exercises such as toe taps, heel slides and pelvic floor exercises. Building strength and muscle bulk in your rectus abdominis and obliques will also help to heal separation and create a stronger abdominal container. Our specialized pelvic floor safe core classes are designed specifically for women with prolapse.
3. Mobility and Posture
It is extremely common for women with prolapse to grip through their upper abdominals, rib cage or even jaw as a protection mechanism. Additionally, new mothers spend so much time in a hunched forward position. Our back pain and pelvic floor safe yoga classes are deigned to help you to release this tension, reduce upper back and neck pain and allow your body to let go and trust.
4. Full Body Strength
Full body strength is vital for women living with prolapse. The stronger your arms, legs, core, and back is, the less load that will be placed on the pelvic floor to do everyday tasks. Our pelvic floor-safe workouts are designed to help you build strength safely and progress from early postnatal workouts to advanced postnatal fitness.
5. Returning to Impact Safely
It is our goal to help you return to the type of exercise you love - and for many women, this means impact. The EMP includes a complete return to running and impact series that is designed to support women in returning to impact and running safely and confidently.
If you are interested in returning to running or impact and want to find out more, please read these two posts:
Returning to Running After Pregnancy - Are you Ready?
Postnatal Return to Running - The Screening Checklist!
Pessaries
A pessary is a medical-grade silicone device that is inserted into the vagina to support the pelvic organs. It is like a ‘sports bra’ for your vagina. Pessaries come in a range of shapes and sizes, so it is essential to have them fitted with the right one for you.
Pessaries are a conservative way to treat prolapse and can be used by the majority of women. It is essential to be fitted for a pessary by a Women's Health Physio or OB/GYN who is trained in pessary fitting. Pessary fitting is achieved through trial and error. Correct fitting should relieve or reduce your symptoms, allow you to void and defecate, stays in place with activity and do not cause pain or discomfort. Most pessaries are designed to be taken in and out by the user (after being fitted for one by a Pelvic Health Physiotherapist or OB/GYN).
Generally, pessarys are well tolerated and can be a great conservative option. One study found that 92% of women reported overall satisfaction, 50% reported resolution of urinary symptoms, and almost all women reported resolution of prolapse symptoms within two months of pessary use. (Clemons et al. 2004) Pessarys, however, do not come without their risks, such as the risk of increased urinary leaking (Occult SUI), obstructed voiding, vaginal infection and vaginal wall erosions, which is why it is important to be correctly fitted and managed by a specifically trained Gynaecologist or Pelvic Health Physiotherapist.
Depending on the type of pessary you are fitted with, you can choose whether to wear your pessary all the time or just for exercise. You can also take it out for intercourse or during menstruation.
Wearing a pessary will not STOP you from strengthening your pelvic floor! Research suggests that wearing a pessary can help reduce intravaginal pressure prolapse symptoms. (Clemons et al.). Research also suggests that wearing a pessary can help to reduce the grade of prolapse by reducing the passive stretch on the ligaments supporting the pelvic organs. *Handa et al.
If you are pregnant and have previously been fitted with a pessary, we understand that you would want to continue wearing it during pregnancy. We recommend speaking with your OB/GYN or antenatal team to see whether wearing a pessary suits you. Anything inserted into the vagina carries a risk of infection, so it is important to ensure you are sanitizing your pessary well and looking out for any changes to vaginal discharge.
Please note that some women may not be suited to a pessary. Women with a hypertonic pelvic floor, vaginismus, levator avulsion, some previous gynaecology surgeries, obstructed voiding, and more severe prolapse symptoms may not be suited for a pessary. This is why it is essential to see a Pelvic Health Physio or OB/GYN to be fitted and discuss whether it is the best treatment option for you.

Pregnancy with Prolapse
We understand just how difficult it can be to navigate your pregnancy with pelvic organ prolapse. You may have already noticed an increase in your symptoms, and you may be wondering just how your body / pelvic floor is going to cope.
We understand the range of emotions you may be feeling about your pregnancy, including fear, anxiety and confusion. There isn't enough information out there to support women who are experiencing pregnancy with prolapse. We hope to change that in the Empowered Motherhood Program.
If you are pregnant with prolapse, we recommend reading our article here on navigating pregnancy with prolapse.
The process of pregnancy itself places a significant load on the pelvic floor. During pregnancy, the levator hiatus (the pelvic floor outlet through which the urethra, vagina, and rectum pass through) increases in width as the muscles of the pelvic floor start to thin and stretch. In addition, there is an increased mechanical load on the pelvic floor from the weight of your baby, the weight of the uterus and placenta and the increased blood volume and body weight.
If you are pregnant with prolapse, we would love to invite you to trial the EMP Pregnancy program. This program includes a series of workouts, pelvic floor exercises, and expert education to help you move safely during your pregnancy and protect your pelvic floor. We will highlight some of our recommended videos in this post so you can understand how the EMP can support you.
Pregnancy and Increase in Symptoms
Your prolapse symptoms of heaviness will likely increase during your pregnancy. This is due to a combination of pregnancy hormones that work to soften and lengthen the pelvic floor, an increased load on the pelvic floor and compromised movement patterns. However, an increase in symptoms (often more noticeable in the first and third trimesters) does not necessarily mean that your prolapse is getting worse.
In addition to the workouts and education videos in the EMP Pregnancy Program, we recommend working with a women's health physio during your pregnancy to stay on top of your pelvic floor.
Prolapse and Subsequent Births
If you have experienced pelvic organ prolapse following birth, it is really normal and logical to be scared of how a second pregnancy or birth is going to impact your pelvic floor. You may feel a deep resistance to pushing or bearing down. You may wonder how your body is going to cope or whether all the hard work you’ve done to heal your body is just going to go to waste.
We know. We have both experienced this ourselves and also supported hundreds of women through pregnancy and birth after prolapse.
However, we wish to assure you that we know from the research that it really is the first birth that has the largest impact and risk of prolapse (9.7 fold risk) and that each subsequent birth carries only a further 1-fold increase in risk (Quiroz et al. 2010)
When it comes to the choice of birth for your subsequent pregnancies, there is no right answer. It is a deeply personal choice and one that we recommend chatting through in-depth with your antenatal health care team and spending a lot of time considering what YOU most want.
We recommend reading our article here on https://www.empoweredmother.com.au/blog/c-section-birth-after-prolapse

Running with Prolapse
It is not uncommon for women with Prolapse to be told not to run ever again, which is possibly an easier option and usually comes from a well-intended place.
Running places a significant demand on the pelvic floor, and a prolapse tells us that your pelvic floor isn’t functioning optimally. So, by telling someone not to run with prolapse, we are potentially protecting her from making her symptoms worse and needing surgery down the track.
However, for many women, running is such an important part of their lives. Some people are wired that they not only want to return to running but NEED to. Whether this be for mental reasons, fitness or daily function (i.e. chasing a toddler/ running for the bus), running can be a non-negotiable.
We believe that almost all women with prolapse can get back to running. It requires a step-by-step whole-body approach, some serious dedication and mindfulness, and expectation setting surrounding distances and frequency, but it is possible.
If you are interested in returning to running after birth and with a pelvic organ prolapse, then we recommend reading our articles here and here on returning to running safely after birth AND working with a pelvic health physiotherapist to help you.
Should I consider surgery?
There may come a point where conservative treatment hasn’t worked for you or your prolapse is causing you significant pain, trouble voiding or defecating or emotional trauma.
Surgery aims to lift your pelvic organ, restore it closer to its optimal anatomical position, and improve the associated symptoms and quality of life. The surgery is not as simple as it may sound, and although, in many cases, it can be life-changing, it is not without its risks and complications.
If you are considering surgery and have already been working with a Pelvic Health Physiotherapist for some time, then the next step would be to seek out the opinion of a specialised urogynaecologist. Historically many of the prolapse surgeries utilised abdominal mesh placed in the pelvic cavity, however resulted in large numbers of complications and subsequently a worldwide class action. As a result, prolapse surgery is now more highly regulated, and careful consideration is given to each individual regarding the necessity and approach that should be taken, with many non-mesh options now available.
We recommend chatting to health professionals and other women who live in your area about their recommendations and learning more about their experiences. It is not uncommon to seek out a few opinions from different surgeons, which can be incredibly helpful in not only understanding the surgery but also further insight into the various approaches for you as an individual.
Summary
We know just how physically and emotionally taxing living with prolapse can be. We have supported hundreds of women through their prolapse recovery, and we understand the time, patience and hard work required. We are here to support you in healing your body in the best way possible with safe physio-led exercise and expert education you can trust.
Through the Empowered Motherhood Program Prolapse Safe Program, we will work with you to help heal your pelvic floor and regain a sense of confidence and control of your body.
Whilst you might not feel like you have time for your own recovery at this stage, there are some simple yet incredibly effective steps you can take. We will show you how you can heal your pelvic floor, strengthen your core and return to exercise in an empowering and nurturing way.
Kimmy and Lyz x
Get your Free Physio-led Pelvic Floor and CoreWorkouts
Download three free videos for either pregnancy or postpartum.