Returning to Running After Pregnancy - Are you Ready?

Running after birth - It can feel heavy, strange and even scary. So why do so many women want to rush back to running after birth? Well, there’s the feeling of freedom of being outdoors and out of the house.
The mental and physical release. The endorphin rush. And of course, the weight loss that often accompanies running.
But before you lace up your trainers and get the jogging pram out - STOP!
We want to make sure that your body is RUN READY! Why? So that you don’t suffer the consequences of a premature return to running, including prolapse (or making your prolapse symptoms worse), incontinence, pelvic pain, and musculoskeletal injury.
How Your Body Changes During Pregnancy and Birth
During pregnancy, the muscles, ligaments and fascia of your pelvis and core undergo a huge amount of change and stretch. Here is a summary of just *some of the ways your body has changed during pregnancy.
Abdominal Changes
You fit a whole human in your belly. It’s no surprise that there have been a few changes.
The linea alba (the band of fibrous connective tissue that runs from your breastbone to your pubic bone) undergoes a huge amount of stretch. As your belly grows, your abdominal muscles move further and further apart. This increased distance between your abdominal muscles and the thinning and stretching of the linea alba is what is often referred to as stomach separation.
When you run there is a large amount of pressure that goes through the core.
If you return to running before your body is ready, you aren’t able to distribute that pressure evenly through your core which can mean increased load through the shins, knees and pelvic floor.
Before planning your return to running, focus on creating a strong and connected core and work towards healing your abdominal separation so that you are able to manage and distribute pressure evenly throughout your core.
EMP TIP: We recommend that you can complete at least Level 3 of our Core Connect Program before returning to running.

Pelvic Floor Changes
During pregnancy, the levator hiatus (the pelvic floor outlet through which the urethra, vagina, and rectum pass through) increases in width as the muscles of the pelvic floor start to thin and stretch.
This happens prior to birth, which is why even if you had a cesarean birth, your pelvic floor will be in a weakened state and your levator hiatus will be wider than what it was pre-pregnancy.
If you had a vaginal delivery, your levator hiatus size would have increased even more during the crowning process. There can also be deeper tearing inside the vagina which is called levator avulsion.
Due to the increase in hiatus size (plus any damage to the pelvic floor during birth), there is less support to the pelvic organs. This means that returning to running before your pelvic floor has had a chance to recover may predispose you to conditions such as incontinence, prolapse, and pelvic injuries.
If you have a well-functioning pelvic floor, when you run, your pelvic floor will activate just before your foot hits the ground.
In the postnatal period, general the pelvic floor reflex doesn’t respond as well. This means that every time your foot hits the ground, you will have a force of 1.6 to 2.5 times your body weight going through a pelvic floor that is functioning sub-optimally.
In the next post, we will show you the steps you need to take to get your pelvic floor strong enough to return to running.
Pelvic Girdle Changes
During pregnancy, the bones in your pelvis widen to create space for your baby to move down the birth canal (whether or not you had a vaginal birth). When the pelvis is wider, the anatomical position of the hip socket is also wider. This changes the whole biomechanics of the hips and glutes.
If your glutes aren’t firing as well as they used to, they won’t provide the same level of support and stability. This can predispose you to injury.
If you are one of the 50% of women who suffered from pelvic girdle pain or pubis symphysis in pregnancy, and you still have symptoms, you are not ready to run.
If you did have PGP + SPD then err on the side of caution. Focus on creating strength and stability around the pelvis through the pelvic floor, core and glute strengthening exercises before returning to running.

Ligamentus Changes
During pregnancy, your ligaments become a lot more stretchy and mobile due to the hormone relaxin. Research indicates that you have increased levels of relaxin until around 3-4 months postpartum.
If you are breastfeeding and don’t have your period back you are also in a low oestrogen state. When you are in a low oestrogen state, things tend to be a bit more mobile which can predispose you to injury or pelvic conditions.
Running Risk Factors
Reading a list of risk factors is never fun. We generally don’t like lists of this kind as they don’t provide you with any guidance on where to go next. If you identify with one or more of the following risk factors, it doesn’t mean that you will never be able to run again.
It just means that you are at higher risk of injury and we just want you to take some extra precautions including making an appointment with a Women’s Health Physio or getting in touch with us for some further advice and recommendations.
This list also doesn’t mean that your body is ‘broken’ or that anything is wrong with you. Pregnancy, birth and motherhood journey can affect us on so many different levels and it can leave its mark in a myriad of ways.
If you tick any of the following boxes, we would recommend waiting to return to running until you have seen a Women’s Health Physio.
- I am less than 3 months postpartum. Recommendation: wait until at least 3 months postpartum.
- I am experiencing incontinence or prolapse-like symptoms (a feeling of heaviness in the vagina). Recommendation: See a WHP or try our Pelvic Floor SAFE Program.
- I suffered from a levator avulsion. Recommendation: See a WHP or Gynaecologist before running.
- I have experienced a third or fourth-degree tear. Recommendation: See a WHP or Gynaecologist before running.
- I have ongoing pelvic or back pain. Recommendation: See a WHP or try our Postnatal Program to help increase strength through core, pelvic floor and glutes.
- I have abdominal separation that is greater than 5 finger-widths. Recommendation: See a WHP or try our Core Connect Postnatal Program.
- I have ongoing musculoskeletal pain. Recommendation: See a physio.
- I am still bleeding. Recommendation: Wait until at least 3 months postpartum - if you are still bleeding after 6 weeks postpartum, please check with GP.
- My stitches haven’t healed well (either C-section or perineal stitches). Recommendation: Please check with GP.
- I have a history of hyper-mobility disorder or connective tissue disorder. Recommendation: Please check with Physio.
- I have been diagnosed with REDS - Relative Energy Deficiency Disorder. Recommendation: Please check with GP.
- I have a history of getting obsessed with running. Recommendation: Chat with your GP and develop a mental health plan if necessary.
- I have a BMI that is over 30. Recommendation: Work with a nutritionist or chat with your GP.
In the next post, we will look at our Return to Running ‘Checklist’ and help to get you run-ready!
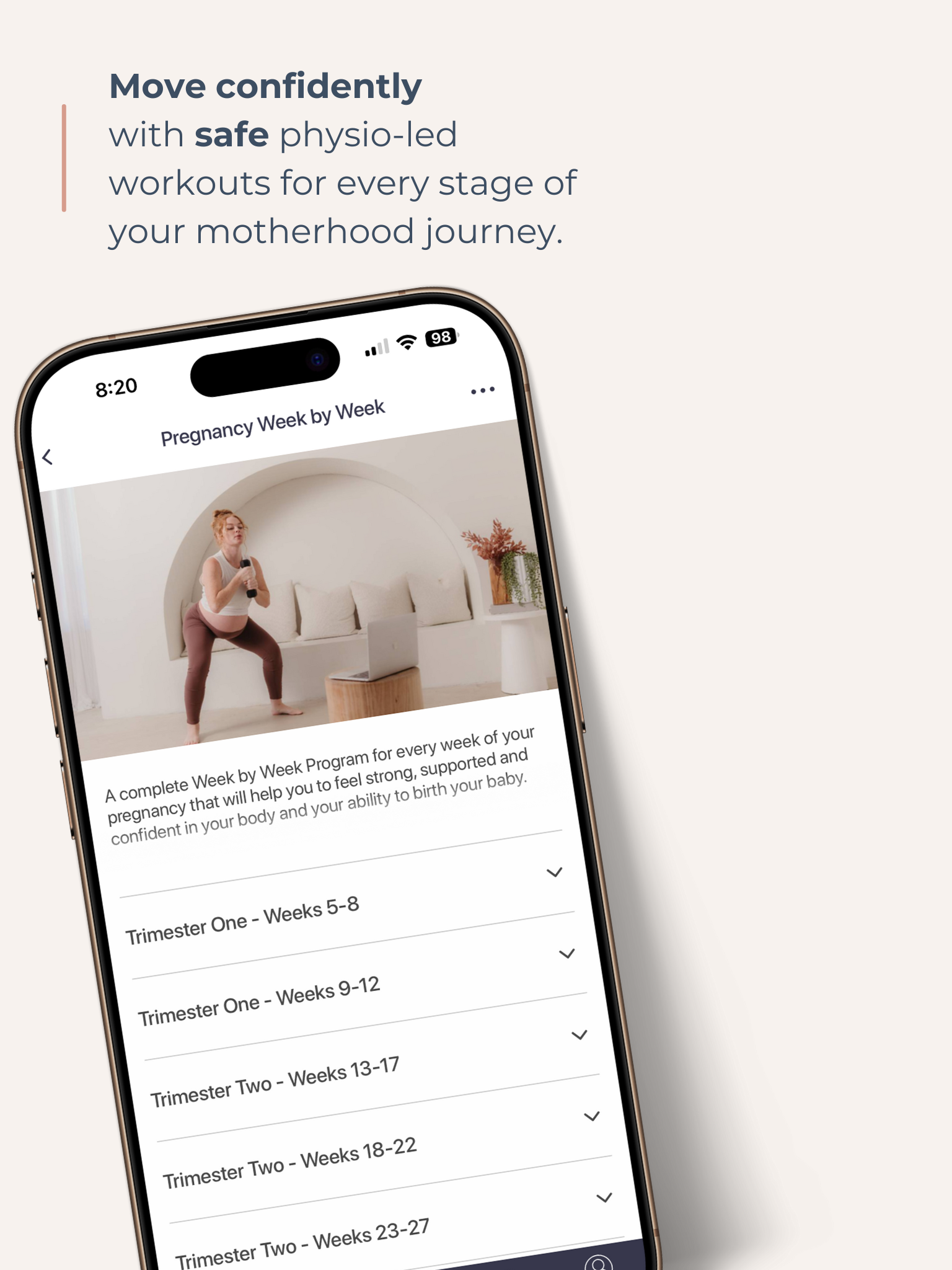
Get your Free Physio-led Pelvic Floor and CoreWorkouts
Download three free videos for either pregnancy or postpartum.