What is PGP Pain? PGP Pain Treatment, Symptoms and Safe Exercise

What is Pelvic Girdle Pain in Pregnancy?
Answer in Brief
Pelvic Girdle Pain (PGP) is discomfort around the pelvis during pregnancy, often affecting the pubic bone, sacroiliac joints, or buttocks. It’s caused by hormonal changes, postural shifts, and muscle imbalances, and can range from mild to severe, impacting mobility. Affecting up to 60% of pregnant women, PGP can be managed with safe exercises, pelvic support, and movement modifications to reduce symptoms .
Key Takeaways
- Pelvic Girdle Pain refers to pain around the pelvis during pregnancy and can present in multiple regions, including the pubic bone and sacroiliac joint.
- Pregnancy pelvic girdle pain is usually caused by changes to your joints, ligaments, posture and biomechanics as your body adapts to support your growing baby. It can range from mild discomfort to significant pain.
- Pelvic girdle pain in pregnancy is common, with up to 60% of pregnant women experiencing mild to moderate pelvic girdle pain at some point in their pregnancy. Wu et al., 2004 > https://pubmed.ncbi.nlm.nih.gov/15338362/
- Approximately 20% of women will experience pain severe enough to require clinical attention. Vleeming et al., 2008 > https://pubmed.ncbi.nlm.nih.gov/18259783/
- PGP typically has an onset between 20-28 weeks gestation (although it can start earlier, especially in second and third pregnancies).
- Common symptoms of pelvic pain include:
- Sharp pain with movements like rolling in bed, standing on one leg, or climbing stairs
- Clicking or grinding in the pubic bone
- Deep aching in the buttocks or lower back
- A shearing or grinding sensation in the pubic bone
- A lot of women get told they just have to put up with pelvic girdle pain; however, this isn’t true. Specific pelvic girdle pain-safe exercise and pelvic support, alongside some simple modifications to your daily movement, can help break the cycle of pain and reduce the symptoms of PGP.

What Is Pelvic Girdle Pain in Pregnancy?
Pelvic Girdle Pain (PGP) refers to discomfort or pain felt around the pelvis, often at the front near the pubic bone, the back of the pelvis at the sacroiliac joints, or deep in the buttocks. It usually shows up between 20–28 weeks of pregnancy, though many women experience symptoms much earlier, especially in second or third pregnancies.
Statistically, 1 in 5 women will experience PGP that is severe enough to impact daily life or require medical treatment. But even milder symptoms affect around 60% of all pregnant women, making it incredibly common, yet still often misunderstood or dismissed.

What Does Pelvic Girdle Pain Feel Like?
No two women experience PGP in the same way, but common symptoms include:
- Stabbing or aching pain in the pubic bone or hips
- A grinding or clicking sensation when walking or turning in bed
- Lower back or deep glute pain, often one-sided
- Discomfort that worsens with activity or after a long day
- Difficulty walking, standing on one leg, or climbing stairs
Why Does It Happen?
Your body undergoes some incredible hormonal, physical, and structural shifts during pregnancy in order to prepare your body for birth. PGP usually stems from three key causes:
1. Hormonal Changes & Ligament Laxity
During pregnancy, your body undergoes extraordinary hormonal shifts to support your growing baby and prepare for birth and breastfeeding. Key hormones like relaxin and progesterone play a crucial role; they soften your ligaments to allow the pelvis to widen in preparation for birth.
This increase in ligament laxity means your pelvic joints may move more than usual. While your pelvis remains strong and stable, this added mobility can sometimes cause discomfort or pain, especially around the sacroiliac joints or pubic symphysis. This is known as pelvic girdle pain (PGP).
2. Postural and Load Shifts
During pregnancy, the lumbar spine region becomes maximally stressed due to large changes in your posture. The main postural changes that occur are:
- Increased Lumbar Curve: The increased weight through the abdomen leads to a more pronounced arch through the lower back. This change typically occurs around 20-30 weeks.
- Widening of the Pelvis: In preparation for birth, the pelvis begins to widen. You may notice you stand with your legs slightly wider, and the weight distribution between your legs can change. This is more pronounced around 30-40 weeks.
- Forward Head and Rounded Shoulders Posture: Increased weight through your abdomen and breast tissue, alongside a shifting centre of gravity, can cause your head, neck and shoulders to round forward, often leading to upper back pain. This is a common experience in the third trimester.
3. Muscle Imbalances
Pre-existing postural patterns, muscle imbalances, old injuries, or how you carry a toddler can all create uneven movement through the pelvis. This increases strain and inflammation. If the core, glutes, or deep stabilizers aren’t supporting the pelvis effectively, the body may compensate in ways that increase stress on the pelvic girdle.
Can Pelvic Girdle Pain Make It Hard to Walk?
Yes. If you have ever experienced pelvic girdle pain, you’ll know that sometimes even walking the shortest distances can feel impossible. During pregnancy, reduced muscular support, changes to connective tissue, and increased pelvic mobility can all contribute to discomfort. Joint instability, muscle guarding (tightness from overcompensation), and poor load transfer across the pelvis make walking challenging. The good news? With targeted, physio-led exercises that focus on restoring balance, stability, and strength, most women can significantly improve their mobility and reduce pain.
How to Relieve Pelvic Girdle Pain Safely
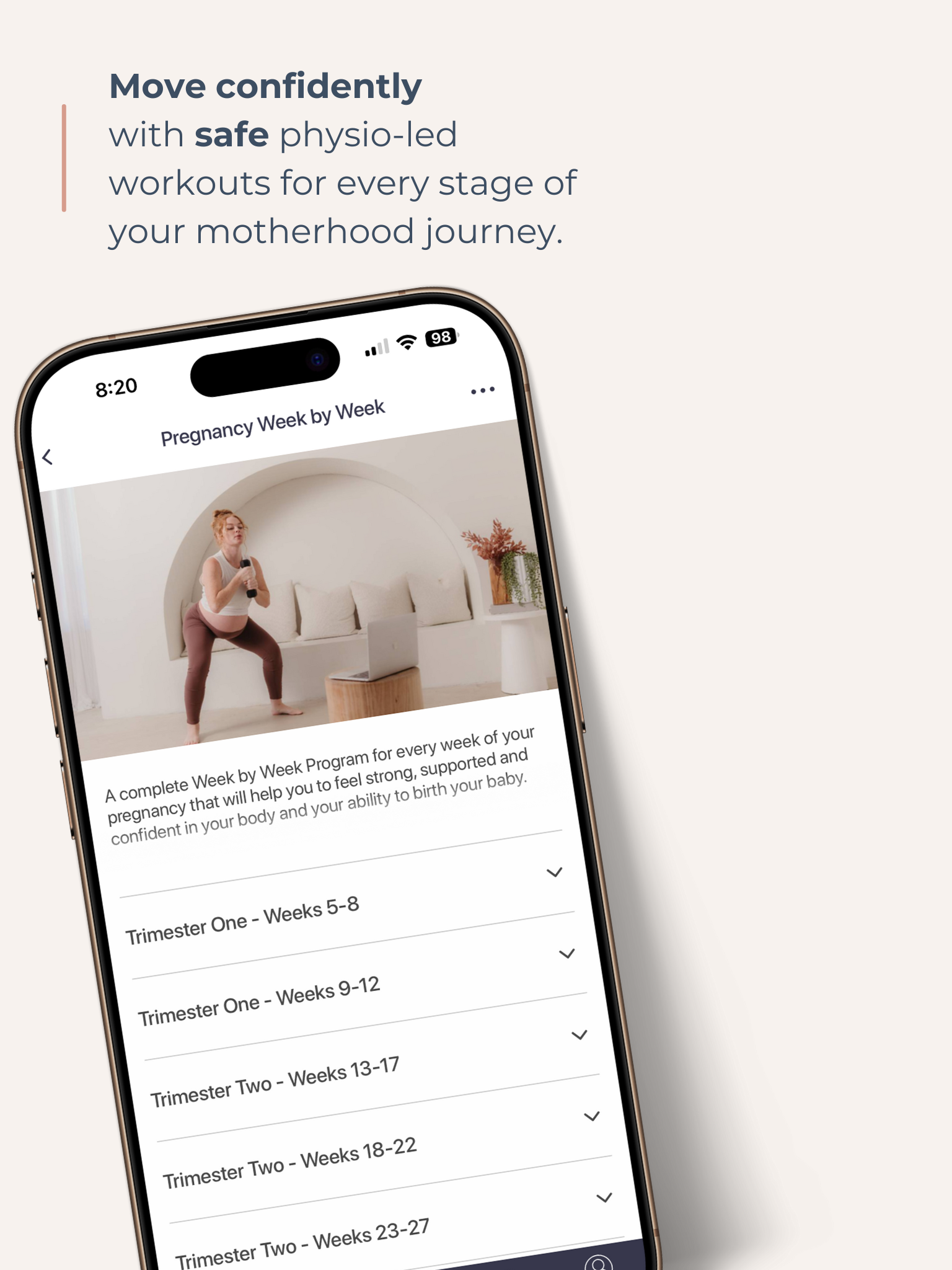
Stopping movement completely can actually make PGP worse. That’s why we created the EMP Pelvic Girdle Pain Safe Program, to help you move safely, reduce pain, and feel supported every step of the way.
Simple, Effective Tips:
- Sit to get dressed, avoid standing on one leg
- Avoid wide stances or deep lunges
- Use a pelvic support belt during activities
- Keep your knees together when rolling in bed or getting out of a car
- Use ice on the pubic bone at night to reduce inflammation
- Gently engage the pelvic floor before moving
- Do short pelvic tilts before standing up
- Use a foam roller or ball to release glute tension
And most importantly: keep moving, but choose the right kind of movement.
Best Exercises for Pelvic Girdle Pain
Safe, physio-led movement can make all the difference. At EMP, we focus on:
-
Glute & Core Strengthening
This helps stabilize the pelvis and reduce joint strain. Think bridges, clamshells, and side-lying work.
-
Stability Over Mobility
Avoid overstretching or open-chain movements. Instead, build control and support with wall sits or supported squats.
-
Low-Impact, Controlled Movements
Pilates, resistance band work, and gentle yoga flow are great for building strength while staying within a safe range of motion.
What Makes It Worse?
Knowing what to avoid is just as important:
- Asymmetrical exercises (like lunges or standing on one leg)
- Prolonged walking or standing, especially on uneven surfaces
- Deep squats or twisting postures
- Carrying weight unevenly (like a toddler on one hip)
- Bucket-style lounge chairs that allow your pelvis to drop
Is Birth Still Possible with PGP?
Absolutely. Most women with pelvic girdle pain go on to have vaginal births. You can prepare by:
- Measuring your pain-free range of movement in advance
- Including that in your birth plan
- Using upright or side-lying positions (instead of deep squat or lithotomy)
- Using props or support under the knees
- If you have an epidural, opting for a supported side-lying position
When Should I See a Health Professional?
If your pain impacts your daily life, limits your walking, or gets worse despite movement adjustments, it’s time to get support. A pelvic health physiotherapist is the best first step. They’ll assess your posture, strength, and movement patterns to create a tailored plan for relief.
Summary
With the right kind of movement and expert guidance, pelvic girdle pain can be managed.
The EMP Pelvic Girdle Pain Safe Program is physio-designed and pregnancy-tested. Whether you’re dealing with sharp twinges, daily discomfort, or uncertainty about what’s safe, we’re here to help you move, feel, and live better.
Get your Free Physio-led Pelvic Floor and CoreWorkouts
Download three free videos for either pregnancy or postpartum.