Returning to intimacy after birth. When pleasure becomes pain....

Written by Katie Stan-Bishop - APA Titled Pelvic Health Physiotherapist
The timing of getting back to intimacy after having a baby is such a personal journey. There is no one ‘right’ time to return to the bedroom after birth - despite many women feeling pressure to return to intimacy after their 6-week check up.
It is important to remember that your journey is unique, and your feelings around birth, your emotional and mental well-being and your physical recovery can impact your own experience.
Transitioning into motherhood is a big (but beautiful) process with significant physical, hormonal and emotional changes. These changes are not always easy to navigate, and naturally, they will impact your desire to have intercourse or even engage in acts of intimacy. Sometimes, we may have reached our limit, and although we may want to engage in intimate activities with our partner, we may feel touched out with nothing left to give.
For some women, the physical activity of penetrative intercourse may cause pain, fear or anxiety. I understand that this can be incredibly concerning and is not the way you want to feel during acts of intimacy. There may also be a significant change to the pleasure you may have felt pre-baby. You are not alone in this; giving yourself the time and space to heal and rediscover what feels right for you is important.
If you are experiencing pain with intercourse following the birth of your child, you are not alone. Research suggests that around 60% of Australian women experience changes in sexual function during the 12 months after childbirth. Openly discussing sex is often considered taboo, and many people feel unable to discuss it with their partner or health practitioners; it is certainly not an ‘easy’ topic to bring up at mothers’ group.
However, as a health professional with a special interest in pelvic pan, one of the things that I would love to reassure you of is that health professionals are trained to listen to and provide advice on managing painful sex. No topics are ‘off-limits. Find a care provider that ensures you have the time to share and holds the space for you. Your GP or obstetrician is a good place to start. They may check for any obvious signs of infection or underlying conditions that may be causing pain. From there, you may be referred to other health professionals such as physiotherapists, psychologists, or sexologists. The ‘source’ of pain can be multifactorial, so your treatment should reflect this.

Why don’t I feel like sex anymore?
Do any of these sentiments resonate with you?
- “I feel like I have just given birth; there's no way I am ready for intimacy just yet.”
- “I am afraid that something is going to break to get damaged if we have sex.”
- “My body looks and feels so different. I don’t feel attractive, which is making me avoid intimacy.”
- “All I can think about is my baby or other children waking up. I can’t relax and enjoy it.”
- “I am so tired. All I want to do when I get to bed is sleep.”
- “My hips, back and breasts hurt. Even if I wanted to, I can’t get comfortable.”
- “I have been needed and touched by little people all day. I don’t have anything left to give and just don’t want to be touched anymore.”
These are just some of the frustrations and challenges I hear in the clinic. There are so many physical and emotional changes that can make intimacy a challenge during the pregnancy and postpartum phases. It is one reason you need a personalised approach with someone who can provide empathy and support during this stage. Some changes that can occur after childbirth include:
- Hormonal changes, sensory overload, pain, tissue recovery, physical trauma, sleep deprivation, vulval changes, and breast changes.
- A new baby's arrival can shift the focus of the relationship as you navigate parenthood together. Added stressors such as work, finances, and lack of sleep can also impact your relationship.
- Changes might include pressures from extended family, differences in parenting approaches, and increased demands from other children.
- Trauma from birth, changes in self-image (including body image), and mental and physical fatigue. There may also be preexisting pain or mental health challenges that also impact your well-being.

How can a Pelvic Health Physiotherapist help to reduce your pain during intercourse?
Your sexual health and well-being are an incredibly important part of your overall health. During your postpartum assessment, your pelvic health may ask about your sexual function and screen for any issues or concerns. This aspect of your recovery is as important as how you feel physically. Your physiotherapist can help by assessing the pelvic floor muscles for any increased tension (which is common after significant life changes like welcoming a baby), examining any scarring from perineal tears or an episiotomy, assessing for sensation changes, and listening to any concerns, fears, or trauma regarding intercourse and orgasm. After a thorough examination, your physiotherapist can provide advice on returning to sexual activity and create an individualised treatment plan to support your intimacy goals.

Pelvic Floor, Birth and Sex
The pelvic floor muscles can be one of the most common culprits responsible for pain with intercourse. Like any other muscle in our body, the pelvic floor needs to be able to contract and relax. A web of fascia, ligaments, and nerves is interwoven within the pelvic floor. For some women, the nerve endings in the pelvic floor may become sensitised, exacerbated by trauma or injury to the pelvic floor. Lower oestrogen levels in the postpartum period can result in dryness and sensitivity, which can occur regardless of the mode of delivery. With low oestrogen levels, the vagina may not produce as much natural lubrication, and the vaginal walls may also be a little stiffer. Hormonal changes can contribute to dryness and sensitivity to the tissue around the vagina and external genitalia, which may also create painful stimuli.

Sleep and Mental Health
In addition to physical recovery following birth, you may also face the added challenge of fatigue and sleeplessness. One of the core things we need to function is sleep, and lack of sleep can impact our mood, which may mean that natural desire and arousal mechanisms have changed. Ongoing adjustments and challenges within intimate relationships can also result in some strain, which may impact sexual desire.
Research also suggests that women who have a history of persistent or chronic pain or trauma (this may be unrelated to birth), may be at risk of experiencing pelvic pain for longer periods in the postpartum period. This may be due to changes in our nervous system that can occur over a long period. This information highlights the importance of psychological support to assist with your mental wellbeing. You can talk to your GP for a referral to psychology or counselling to provide professional support.
Some Tips on Navigating a Return to Intimacy
- Talk with Your Partner: If you are experiencing pain or anxiety regarding sex, it may be helpful to communicate these feelings to your partner. In the process of healing pain, it’s important that you feel secure, safe, and supported. Open conversations about your thoughts and feelings, along with agreeing on some strategies together can make a big difference to your recovery.
- Lubrication: Due to the hormonal changes that take place following birth, you may need to use more lubrication during intercourse. Using a water-based or hybrid lubricant is recommended, as well as choosing a good quality brand with minimal colour or fragrance.
- Pelvic Floor Rehab: If you have a non-relaxing pelvic floor or painful trigger points, you may need to work with your physiotherapist. This work may involve strategies such as manual release, stretches, and home exercises to improve awareness and coordination. Your physiotherapist will also help reduce the severity of painful scar tissue through desensitisation processes and scar tissue massage, which you may be shown how to perform at home.
- Prioritise Your Mental Well-being and Sleep: If you are struggling with any aspect of your mental health and well-being after having a baby, for whatever reason, try to make it a priority to address this. There is growing research suggesting that those with pre-existing pain, fatigue, and previous trauma may be at increased risk of developing persistent pain in the postpartum period. Seeking specific help to support your mental well-being is important.
- Explore Intimacy and Pleasure: If you have the opportunity, adding in foreplay and lots of outercourse can be a great starting point. It’s important to remember that intimacy doesn’t have to equal intercourse. Allow time and space for your body and mind to get into the mood, which may increase natural lubrication. Intimacy that results in pleasure, not pain, even if it doesn’t involve penetrative intercourse, is really important. You can also try positions where you can control the depth and speed of penetration, with some positions allowing your legs and hips (and pelvic floor muscles) to be more relaxed.
About the Author - Katie Stan-Bishop
Katie holds a post-graduate Master's qualification in Continence and Pelvic Health Physiotherapy and is a titled Men's, Women's Health, and Health Physiotherapist, as awarded by the Australian Physiotherapy Association. In addition to Pelvic Health qualifications Katie has also undertaken extensive education in the field of pain and pain science.
Katie is the founder of Katie Stan-Bishop Physiotherapy and works in Albany, WA. Katie is passionate about treating pelvic pain and empowering both men and women to live a life free from pain. Her other expertise includes managing bladder and bowel leakage, pregnancy and post-pregnancy care (including return to exercise), and prolapse, with qualifications in pessary fitting as part of prolapse management. Katie is committed to ongoing education and training to continue providing expert advice to her clients and the wider community.
Katie’s passion for rural health drives her commitment to providing high-quality care in her community. Our rural communities face unique challenges, and it is imperative that these are considered when delivering advice and management to clients.
Follow Katie on Instagram katie_pelvic_physio
References
Alligood-Percoco, N. , Kjerulff, K. & Repke, J. (2016). Risk Factors for Dyspareunia After First Childbirth. Obstetrics & Gynecology, 128 (3), 512-518. doi: 10.1097/AOG.0000000000001590.
Cattani, L., De Maeyer, L., Verbakel, J. Y., Bosteels, J., & Deprest, J. (2022). Predictors for sexual dysfunction in the first year postpartum: A systematic review and meta‐analysis. BJOG : An International Journal of Obstetrics and Gynaecology, 129(7), 1017–1028. https://doi.org/10.1111/1471-0528.16934
Marvi, N., Heidarian Miri, H., Hooshmand, E., Abdollahpour, S., & Zamani, M. (2021). The association of mode of delivery and dyspareunia: a systematic review and meta-analysis. Journal of Obstetrics and Gynaecology, 42(3), 361–369. https://doi.org/10.1080/01443615.2021.1916802
McDonald, E. A., Gartland, D., Small, R., & Brown, S. J. (2016). Frequency, severity and persistence of postnatal dyspareunia to 18 months post partum: A cohort study. Midwifery, 34, 15–20. https://doi.org/10.1016/j.midw.2016.01.012
NICE Guideline NG 194. Post Natal Care perineal pain. Evidence review underpinning recommendations 1.2 15 to 1.2 22 April 2021
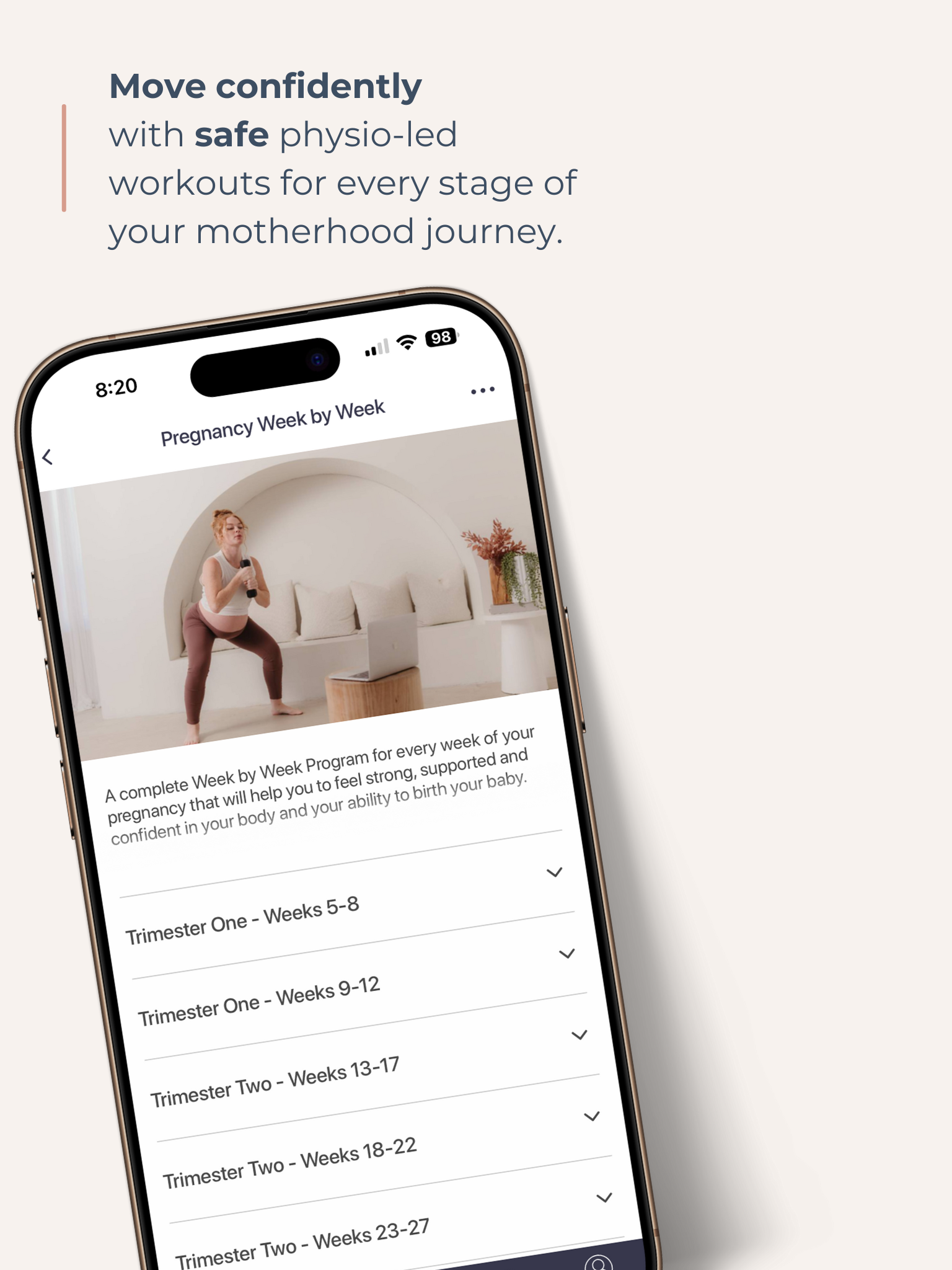
Get your Free Physio-led Pelvic Floor and CoreWorkouts
Download three free videos for either pregnancy or postpartum.