Lyz's Birth Story - A Maternal Assisted C-Section Birth

On the 1st day of May, we welcomed our third child into the world. My daughter Isabelle Florence was born by Maternal Assisted Caesarean Section (MAC) and it was such a magical and empowering birth.
In this post, I want to share the story of Isabelle's birth, as well as some more information about MAC births, including the steps I took to prepare and the behind-the-scenes details of what happens in a MAC. I hope that through sharing my experience that it helps more women and partners feeling informed, and can provide some reassurance that a C-Section birth CAN be beautiful and empowering.
What is a Maternal Assisted C-Section?
A maternal-assisted C-Section birth is a caesarean section delivery that allows the mother to be actively involved in her birth. In a maternal assisted caesaren (MAC) the mother is able to reach down to help pull her baby out of the womb, lifting the baby straight onto her chest for skin-to-skin contact.
Before I dive in further to my personal experience, it's important to recognise that a MAC birth is not an option for all women.
There are a number of factors to consider, with the health of the baby and the mother being paramount, as well as hospital policy and Obstetrician experience. A MAC is a relatively new type of birth that has yet to become a common practice in Australia, so it is something that has to be discussed in detail with your medical professional. There are many instances where a MAC is not appropriate for medical reasons, such as low-lying placenta, twins, breech presentation, preterm baby, and preeclampsia, and it is not possible in an emergency caesarean. This is not an exhaustive list, and any woman interested in a maternal-assisted caesarean will need to be assessed on an individual basis. It is also important to be aware that a MAC is not for the faint-hearted, so if you struggle with the thought of surgical incisions and blood, a MAC birth may not be for you.
Preparing for a Maternal Assisted C-Section
The first step in my preparation was to ask! I was familiar with the concept of a MAC from my work in Women's Health. However, I knew that a MAC isn't yet common practice in Australia. Although my Obstetrician, Dr Lynn Townsend, had not previously performed a MAC, I was incredibly fortunate that she was open to exploring the option with both myself and the hospital, as she appreciates the importance of trying to support a woman in her birthing choices.
Having a maternal-assisted C-Section Birth meant that I was a part of the medical process, and as such, I had to prepare for it. In the weeks leading up to the birth, we discussed the logistics of the birth, the importance of ensuring a sterile environment, and the steps involved. One of the main concerns with a MAC is the risk of introducing bacteria into my abdomen due to the mother's hands entering the surgical field. This could ultimately result in a serious infection, which is why ensuring we both felt confident in all the steps required to keep the environment sterile was important.
We practised how to do a surgical hand wash, putting on a gown and sterile gloves in the theatre whilst I was lying on my back. We rehearsed the timing of when I would reach down to deliver my baby from the abdomen and the speed at which I would lift her to my chest to ensure Dr Townsend had enough time to check that the cord had enough length to it whilst it remained in my uterus.
Dr. Townsend also discussed with me that although we were aiming for a MAC, if the birth changed course, the baby was distressed, or I went into spontaneous labour, a MAC would not be possible. We discussed all of the usual risk factors of caesarean and vaginal birth (in my case, a VBAC), and I consented to both modes as I was preparing for both.
In the week before the MAC I talked through with my husband all of the steps involved in the MAC, so that he knew his role and what to expect. He had been present and involved in both our previous births and was proud of me for wanting to be more involved.


Birth Day - Preparing for Surgery
The day is here! Whilst it has been incredible to experience pregnancy one final time, I won't lie, I'm delighted to be at the end of the pregnancy and am unbelievably excited to meet the final piece to our family puzzle.
My MAC is scheduled for 9am, so I arrive at the hospital at 7:30 am. I am greeted by the friendly midwives who then organise a few assessments such as blood pressure, anesthetist consults and I am cannulated to take pre-op blood work. My jewellery is removed, I'm given compression socks and a gown to put on, and my husband puts on scrubs.
Once this is all complete, I am then wheeled on my bed to the theatres with my husband walking next to me. It is all starting to feel very real!

Spinal Block time
Once we arrive at the pre-theatre bay, I am instructed to do a very thorough hand wash and not to touch anything unnecessarily. It feels very clinical, cold and I'm starting to get a little nervous.
The anaesthetist, Dr. Jenny Kaldor, arrives, which means it's spinal block time!I am asked to sit on the edge of the bed, my gown is open so she can see my spine, and my back is painted with a betadine solution to ensure a clean environment. Once this is done, a local anaesthetic is injected into the area so that when the larger spinal block needle goes in next it is not as painful. I am told to hug a pillow and hunch over to curve my spine as much as I can, to open up the space between the vertebra.
The first attempt at a spinal block is made, but OUCH, it is WAY too painful. The anaesthetist gives me more local, and thankfully, the second attempt of the spinal block is much more bearable. It feels like an electric shock in my spine for a split second, followed by a bizarre feeling of pins and needles and warmth gradually travelling down my legs.
The anaesthetist and surgical nurse then lowered me onto my back before the numbness in my lower body really set in. Fairly quickly, I can't move my legs, and I feel quite overwhelmed with this complete feeling of paralysis. Even though I know it is part of the process, and I've experienced it before, it is still quite an overwhelming feeling.
I could have easily gone into a state of panic here, so I concentrated on my breath and calming my nervous system down. I squeeze my husband's hand at this point to let him know I need his support to keep me calm. I am relieved that I have prepared for this birth just as I would have prepared for a vaginal birth. My breathing and mantras are coming in handy.

Time to enter the Theatre
Once they are confident that the spinal block is effective, I am then wheeled into the surgical theatre. My husband stays in the holding bay whilst the final part of the preparations occurs.
I am shifted via a sliding mat across to the operating table. I feel vulnerable, unable to move my legs, and with lots of faces around. Fortunately, they are all smiling and introducing themselves to make me feel as comfortable as possible. The next step is the insertion of a catheter, which I'm grateful not to feel due to the spinal block. Next, My Obstetrician puts antiseptic on my hands, a sterile surgical gown, and sterile gloves. I am told to keep my hands in on my chest and not touch anything, and my husband is then brought into the theatres.
It's at this point that I start to feel a little spaced out. My hands are quite tingly and I'm numb up to my nipple line. I don't like this feeling at all, so I do a meditation to stay calm and connected to my body. I try to relax into the process as much as possible, I know that this is just an effect of the medications in the spinal block. I am so close to meeting my baby, and my husband squeezes my shoulder to let me know he is here.
As soon as my birth team is happy that everything is ready, the energy in the room changes. The playlist we have selected is put on and everyone can feel the anticipation and joy as we are about to birth our baby.
The first incision
One huge difference of a maternal-assisted c-section is that there is no surgical drape dividing us from the Obstetricians. This means that both my husband and I can see the entire operation. I know that this can often be confronting for a lot of people, but for others, it can be empowering. (This is also an option to discuss for normal CS if you wish to see a little more).
My abdomen is painted with chlorhexidine to clean the area, and then the first incision is made! My husband doesn't love the open abdomen view, so he chooses to sit down next to me and wait to stand up until it's time to birth our baby. Being comfortable with watching a C-Section being performed on yourself or someone you love is something that I recommend discussing with your partner and birth team if you are considering a MAC. From where I was lying, I could only see the top part of the surgery, so I chose to watch it in the reflection of the light on the roof! This definitely isn't everyone's cup of tea, but it is something I feel very comfortable with and enjoy.
The team talks us through what is happening as it is occurring, which helps us to feel involved and calm. Once the skin, fascia, adipose tissue, muscle layers have been cut through, the final incision into the uterus and amniotic sac are made, and it's time to meet our baby.
Bringing my daughter into the world
Dr. Townsend and the assisting Obstetrician need to assist to get my baby out to the point from which I can lift. Babies often get quite stuck and need some significant manual help. It can often look quite rough and can be difficult to watch, but babies cope very well, and are designed to withstand the strong contractions from a uterus!
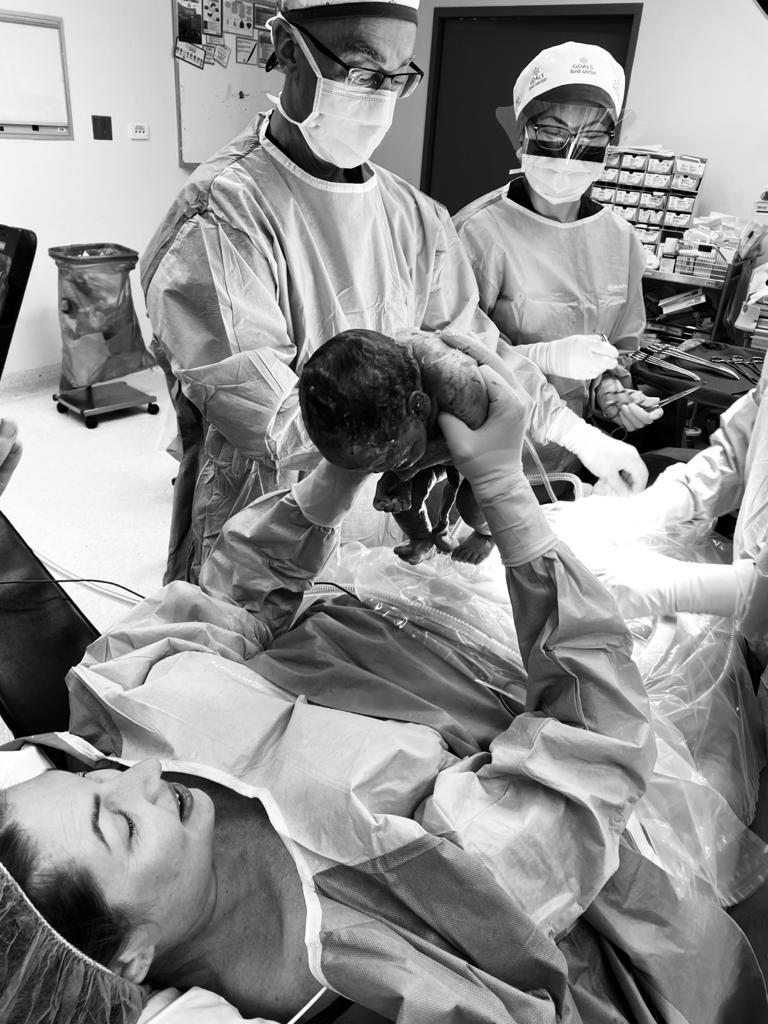
Once Dr Townsend has ensured there are no complications, I am told it's time to reach down. It's the moment we have been waiting for, time to lift our baby into the world.
This moment is one I will never forget. I reach forward to bring my daughter into the world, it is absolutely magical.
I lift the baby up onto my chest, and I'm overcome with emotion, that we completely forget about finding out if it is a girl or boy. My husband checks, It's a GIRL! Whilst I would have been happy either way, this just feels so incredibly special to be able to give my daughter the sister she has been hoping for!
Skin to skin cuddles with my baby girl
One benefit of a maternal assisted C-Section is that you have instant skin-to-skin contact (although in the moment we actually forgot to pull my gown down and gloves off so it wasn't exactly the skin-to-skin moment I had planned, but it was still intimate and beautiful). This is also an option for general C-Section births if you and your baby are ok and is something most hospitals are moving towards... if you ask!
Relief. Joy. Pure love. That mix of emotions when you finally get to hold your baby is magic. My daughter is immediately calmed by my voice and it's such a special moment to share with my husband. Our baby is here, she is safe and I helped to lift her into this world. I cuddle my daughter whilst delayed cord clamping occurs, and my husband cuts the umbilical cord.

Immediately Post Birth
After a few minutes, our daughter is checked by the paediatrician and we are reassured that she looks well and healthy. My gown and gloves are taken off so that when my baby girl is handed is back to me we can have more skin-to-skin cuddles. Whilst we are in our blissful bubble, the team delivers my placenta and my abdomen is sutured back up. I have 200mL of blood loss which is not a lot. There are 6 layers of tissue that require suturing after a c-section which is just one of the reasons why I will feel so sore and tender over the next few weeks.
I'm then taken to the recovery rooms, which is where I manage my first breastfeed. I will never tire of watching the instinct that a newborn baby has when it seeks out to find the breast and knows how to suck.
Introducing - Isabelle Florence 💫
Welcome to the world Isabelle Florence. 3.07KG and 48cm of perfection. After being in recovery for about an hour I am then taken to the ward with Isabelle on my chest and my husband walking next to me. I feel incredibly tired and spaced out from the medication, so I have a nap as soon as I get back to the rooms. My husband is delighted to have some special 1:1 time whilst I nap.
When I wake, I realize how difficult for me to move and position myself to feed Isabelle as I am still numb from the waist up. I don't like this feeling and just want the spinal block to wear off, but know I have to be patient. I keep trying to wiggle my toes, and after a few hours, I can slowly feel the sensation and movements in my legs returning.
Our Family of Five
 Later that afternoon it's time for Isabelle to meet her brother and sister. Watching these first cuddles is truly special and at that moment I know how lucky we are to have been fortunate to bring a third healthy baby into the world. Our family is now complete.
Later that afternoon it's time for Isabelle to meet her brother and sister. Watching these first cuddles is truly special and at that moment I know how lucky we are to have been fortunate to bring a third healthy baby into the world. Our family is now complete.

Thank you to my incredible birth team
I am so grateful incredibly grateful to the birth team who made my maternal assisted c-section possible. I do not have the words to describe how thankful I am to my obstetrician Dr. Lynn Townsend who despite never having performed a MAC was happy to challenge the norm, adopt a new practice and ultimately help me achieve the birth I wanted. And what's even more amazing is since my birth, she has begun offering MAC to many more mums who are appropriate.
Thank you also to Dr. Matthew Peres, Dr. Jenny Kaldor, Midwife Polly Rhydderch, Pediatrician Dr. Parag Mishrag and of course my husband my partner Justin. Every single one of you played an important role in one of the most unforgettable moments of my life and I am eternally grateful.
I also need to give credit to Dr. Jenny and Polly for their birth photography and videography skills. They managed to capture the essence of the birth, so beautifully.
A MAC, THE WAY FORWARD.
I hope by sharing my story, that it helps more women and health professionals to know that a MAC is a possible birthing option. I truly believe that a MAC is the way forward and would love to see it becoming an option as a part of standardised care in Australia. A MAC can make a caesarean far less clinical, more intimate, and more empowering, especially for those who wanted a vaginal birth but for medical reasons we're not able to.
If you are interested in having a MAC, then I encourage you to take the first step that I did. ASK THE QUESTION! Like any change in standard practice, things only change when it is made apparent that women want a change! It will take time, but for every woman that uses her voice in an educated and respectful way we are one step closer to having more positive birth experiences for all women, which as a Women's Physio is something I feel incredibly strongly about.
The Empowered Motherhood Program
If you wish to learn more about recovering from a Caesarean or becoming more informed when it comes to pregnancy, birth, and the postnatal period, I would love for you to have a look at the Empowered Motherhood Program. This is an online expert-led program I have co-created to help better prepare the mothers of Australia.
Get your Free Physio-led Pelvic Floor and CoreWorkouts
Download three free videos for either pregnancy or postpartum.