A 10 hour return trip to see a specialist - Navigating Healthcare Challenges in Rural Australia

Written by Katie Stan-Bishop - APA Titled Pelvic Health Physiotherapist
http://www.katiepelvicphysio.com.au
Growing up on a farm in rural Western Australia shaped much of who I am today. A trip to town was an hour round trip, and it would take us five hours to drive to the nearest capital city. After finishing high school, I moved to the closest city to study. Later, after travelling overseas, my husband and I decided to return to our coastal hometown to raise our children. I have done all my postgraduate studies in my hometown, which was a challenge, juggling work, motherhood, and travelling to the city for practicals. As my career progresses, I am passionate about not just advocating for optimal service provision in our regional and remote areas but also equipping my clients and others with the knowledge that allows them to seek help and problem-solve some of the challenges.
The Reality of Rural Healthcare
Around seven million Australians, 28% of the population, live in rural and remote areas (Australian Bureau of Statistics, 2023). While these regions are diverse, the challenges their residents face are remarkably similar: fewer healthcare providers, greater distances to access care, and limited resources. Whilst these figures sound harsh and the challenges are real, they also present lots of opportunity. Healthcare providers can make a real difference.
As a healthcare provider working in rural Australia, I see firsthand the need for adaptability. Planning, communication, shared care, and providing flexibility in how treatment is delivered can be the difference between a good outcome and a great one.
Unique Challenges in Rural Healthcare
1. Distance and Travel
Long distances to healthcare facilities are one of the most prominent barriers. I have referred clients to specialists, only to realise the trip would mean a 10-hour return journey. That is not just time away from work or family; it is also a financial burden when you factor in fuel, accommodation, and other travel costs. Often, trips to the closest town or capital city need to be planned well in advance and fit in with other appointments simultaneously.
2. Specialist Shortages
Access to specialist services such as Gynaecology may often be unavailable, or there may be long waitlists for public services. For many regional and remote centres, attracting qualified and experienced health care workers is a challenge. The areas that the health professionals service are quite vast, and for many, the wait time for a review may be up to years, with no option of private services without needing to go to the city.
3. Privacy in Close-Knit Communities
In small towns, privacy can be a significant concern. It is not uncommon for people to hesitate to seek care for sensitive issues, like pelvic health, out of fear of gossip or judgment. Understandably, you may not wish for your pelvic health physio to be a fellow mum on your child’s soccer team or to meet them in the school car park. Rest assured that as a pelvic health physiotherapist, I take the privacy and dignity of my clients very seriously. When it is our everyday job, we can switch to professional mode, and our only concern is providing high-quality treatment. Your physio is certainly not judging whether or not your have shaved your legs or have matching socks.
4. Financial and Time Pressures
Rural life often demands prioritising immediate needs, particularly during busy periods like harvest or shearing. In these times, a trip to town can feel like a luxury. Many clients have told me they want to attend appointments but simply cannot justify the time away from the farm or family commitments.
5. Limited Awareness and Conversations Around Health
In rural communities, open discussions about health are rare. The men and women in our rural communities have faced hard and unpredictable challenges, and are extremely resilient. There is a tendency to ‘get on’ with things without complaint. Whilst this can build character, there can be a lack of awareness that comes with less shared experience and, on occasion social isolation.

How We Can Bridge the Gap
While the challenges are significant, they are not insurmountable. Over the years, I have seen how thoughtful strategies can improve access to healthcare, even in the most remote areas.
1. Telehealth
Telehealth has been a meaningful change for rural communities. Clients can receive assessments, exercises, and guidance through video consultations without leaving their homes. While some conditions require in-person visits, telehealth provides an excellent alternative for ongoing care, reducing the need for travel. Many of the local hospitals are now able to delivery the ante natal birth education via telehealth, which has improved the access for so many women.
2. Building Local Networks of Care
Local healthcare providers like GPs, nurses and physiotherapists are often the first point of contact for rural residents. By fostering strong relationships with these professionals, we can create a more integrated approach to care. For example, local providers can identify issues early, offer initial support, and refer clients to specialists when necessary. With proactive clinicians and early detection, preventative treatments can be very effective.
3. Online resources
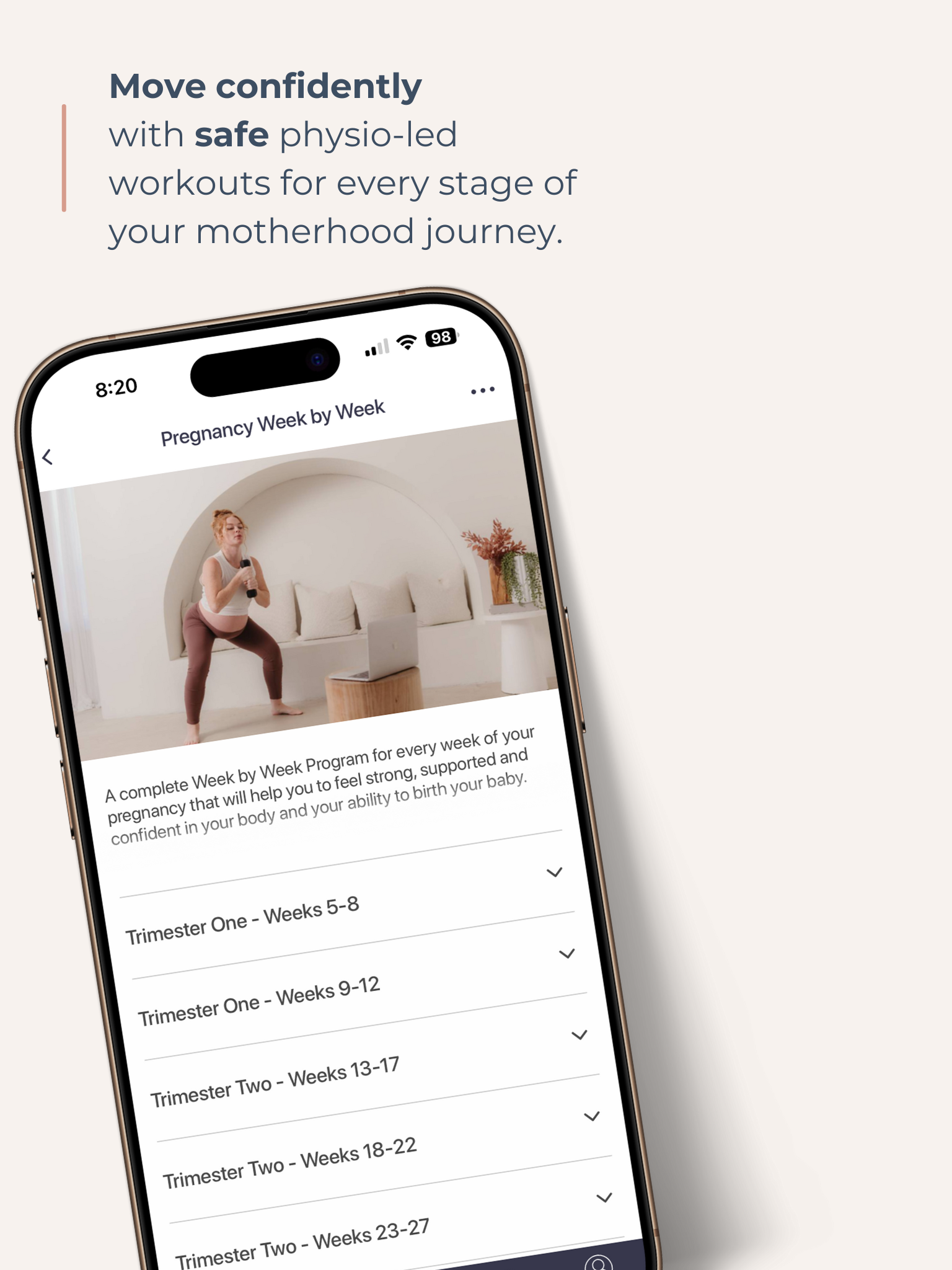
For many of my patients, it may not be possible or viable to join in a group program or access regular physiotherapy for follow-up appointments. I have been utilising online exercise and education platforms such as the Empowered Motherhood Program for many years, as it can assist with providing women with a sense of belonging, commitment and accountability that they may otherwise be missing.
They also have the benefit of being able to access expert-led content daily rather than having to wait for appointments to seek safe movement or education.

4. Education and Awareness
Breaking the silence around health issues is crucial. Workshops, community talks, and even social media campaigns can help normalise conversations about health. In my own practice, I have seen how education empowers people to seek help and realise they do not have to suffer in silence. I have spent several hours traveling to deliver education talks to rural communities. I have witnessed my colleagues effectively deliver outreach services, where they drive or fly to remote communities to offer services on an ongoing basis.
5. Financial Assistance Programs
Travel assistance programs can ease the financial burden of accessing specialist care, but they are often underutilised due to a lack of awareness and fluctuating funding levels. Educating rural residents about these programs can make a significant difference.
6. Supporting Community Connections
Rural communities are built on strong social connections. By leveraging this strength, we can create informal support networks that reduce stigma and encourage people to seek care. For example, local mums’ groups or fitness classes can be safe spaces to discuss health concerns and share resources.
Living in a rural area should not mean settling for inadequate care. With telehealth, community support, and increased education, we can overcome many of these barriers and ensure that everyone, regardless of location, has access to the care they deserve. If you live in a regional or remote area and are struggling to access the care and support you need, do not hesitate to reach out to your nearest service provider. You may be surprised at the level of innovation we now have available to us in service provisions and how passionate healthcare workers are about providing high-quality healthcare.

About the Author - Katie Stan-Bishop
Katie holds a post-graduate Master's qualification in Continence and Pelvic Health Physiotherapy and is a titled Men's, Women's Health, and Health Physiotherapist, as awarded by the Australian Physiotherapy Association. In addition to Pelvic Health qualifications Katie has also undertaken extensive education in the field of pain and pain science.
Katie is the founder of Katie Stan-Bishop Physiotherapy and works in Albany, WA. Katie is passionate about treating pelvic pain and empowering both men and women to live a life free from pain. Her other expertise includes managing bladder and bowel leakage, pregnancy and post-pregnancy care (including return to exercise), and prolapse, with qualifications in pessary fitting as part of prolapse management. Katie is committed to ongoing education and training to provide expert advice to her clients and the wider community.
Katie’s passion for rural health drives her commitment to providing high-quality care in her community. Our rural communities face unique challenges, which must be considered when delivering advice and management to clients.
Follow Katie on Instagram katie_pelvic_physio
Get your Free Physio-led Pelvic Floor and CoreWorkouts
Download three free videos for either pregnancy or postpartum.